Do you wonder why you can’t just “get over” something that happened years ago? This can be a sign that your trauma is still looking for a way out. This guide can help you choose your healing journey and access trauma-informed treatment.
Take a childhood trauma test first to understand whether an early life traumatic event is influencing your mental health today.
What is Trauma Therapy, and How Does it Work?
Trauma therapy is a psychotherapeutic method for treating the effects of psychological trauma. With the support of a mental health clinician, trauma survivors can recall and reinterpret past trauma in a safe and supportive environment. The trauma therapist helps a person express previously suppressed emotions, change beliefs associated with the trauma, and restore a sense of safety and trust in the world.
According to the research of the American Psychological Association, the most popular trauma-focused therapy methods include talk therapy, cognitive behavioral therapy, EMDR, and art therapy.
Understanding Different Types of Trauma Therapy for Complex Needs
Complex trauma, often known as C-PTSD, is the term used to describe trauma that is a sequence of multiple experiences rather than a single event. These layered experiences require a therapy plan that moves in specific stages, starting with physical stability rather than diving straight into the person’s troubled past.
According to research, effective recovery combines different tools, using methods like DBT to stabilize daily crises first, then moving into specialized methods like EMDR to address the underlying root causes.
Expert Insight
Clients with complex needs benefit most from an integrative approach rather than a single modality. Combining relational, trauma-informed work with somatic and nervous-system–based therapies helps address both the emotional meaning of experiences and the body’s learned patterns of protection. An integrative approach is effective because it can foster safety and enhance self-awareness while gently expanding a client’s capacity to tolerate emotions and stress. What matters most isn’t the technique alone, but the flexibility to tailor therapy to the whole person and adjust as their needs evolve.
Rychel Johnson
Mental health professional
6 Evidence-Based Trauma Therapy Methods
Because everyone processes distress differently, there are several distinct therapeutic approaches to treating trauma.
1. Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
Designed primarily for children and teenagers, this approach equips a young person with the tools to manage intense emotions after a traumatic event. It helps kids realize that while they can’t change what happened, they can change how much power that event has over their future. This usually focuses on three main areas:
- Regaining control over the body. Children frequently lack the vocabulary to describe “anxiety.” However, they are aware that their stomach hurts or their heart is racing. TF-CBT teaches them relaxation techniques to reduce physical stress.
- The trauma narrative. Together with a mental health professional, a person creates a book, a drawing, or a poem that tells the story of what happened.
- Parental involvement. Parents or caregivers learn the same coping skills so they can support the child at home.
2. Cognitive Processing Therapy (CPT)
People who have experienced trauma may develop negative beliefs about themselves and the world. For example: “I am such a failure,” “The world is cruel and unfair,” or “I hate people.” These beliefs can harm their self-esteem and relationships, making them feel worthless or think, “Nobody likes me.”
During cognitive processing therapy, people learn to identify and analyze these maladaptive thoughts:
- How valid and constructive are they?
- What feelings and actions underlie them?
Together with a trauma therapist, a person can develop more adequate rational beliefs to replace negative ones. This helps to change the attitude toward the world, moving toward an awareness of one’s own strength and inner resources.
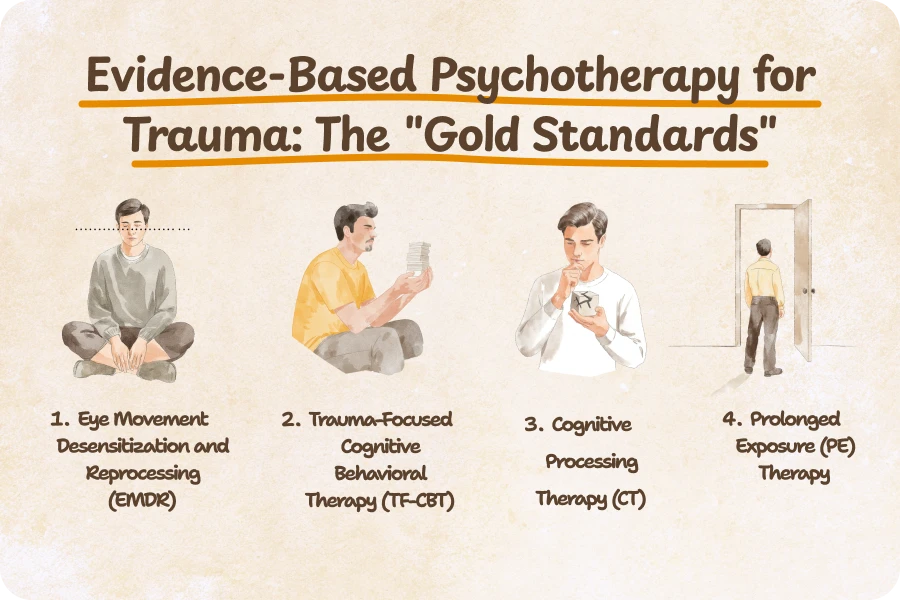
3. Prolonged Exposure Therapy (PE)
The prolonged exposure therapy is built on two main pillars:
- In vivo exposure. Under the guidance of your therapist, you gradually start doing things you’ve been avoiding, like driving over a certain bridge or sitting in a crowded cafe.
- Imaginal exposure. This is where you talk through the traumatic event in the present tense. When you recount the story repeatedly, the memory eventually loses its power to overwhelm you.
In Prolonged Exposure (PE) therapy, grounding is especially important. Grounding refers to skills that help you stay aware, and connected to the here and now, especially when strong emotions or trauma memories arise. These techniques can include focusing on your breath, noticing physical sensations, or using your senses to anchor yourself in the present moment. Being able to ground yourself helps prevent overwhelm and reduces the risk of dissociation during exposure work.
If you want to learn how to ground yourself, Breeze may come in handy. Positive affirmations in the app can help you practice gratitude and self-care:
- “Calm and consistency help my nervous system feel safe.”
- “Regulation is a skill I can practice.”
- “This moment will pass.”
- “I don’t have to decide anything right now.”
- “My needs matter, even when I’m still learning what they are.”
- “Calm does not mean something bad is coming.”
- “I’m allowed to change my mind.”
- “My reactions make sense given what I lived through.”
- “I can release shame that never belonged to me.”
- “No is a complete response.”

4. Narrative Exposure Therapy (NET)
NET was originally designed to help people who have survived long-term stress, like those living in refugee camps or conflict zones, or experiencing repeated sexual assault.
For many survivors, trauma feels like a chaotic internal secret. NET helps turn that experience into a meaningful story. It’s a high-intensity approach, but for those who feel their identity has been swallowed by their past, it offers a way to reclaim the narrative of their own survival.
In a NET session, you literally map out your life. You use a physical string or ribbon to represent your “lifeline.” Along that line, you place stones representing traumatic events and flowers symbolizing moments of joy, connection, and strength. You work with the therapist to turn your memories into a formal “biographical narrative.” By the end of treatment, you have a written document of your life.
5. Dialectical Behavior Therapy
Originally developed for people with intense personality traits and chronic suicidal thoughts, it has become a gold-standard treatment for anyone whose trauma shows up as “emotional dysregulation.”
The word “dialectical” sounds academic, but it just means that two opposite things can be true at the same time. In this case, you are doing the best you can, AND you can do better.
DBT is well-structured. It’s focused on four specific skill sets:
- Mindfulness. Learning how to live in the present moment without immediately judging it or trying to escape it.
- Distress tolerance. It gives you ways to survive a crisis, like a panic attack or a self-harm urge, without making the situation worse.
- Emotion regulation. Think of this as learning how to get out of your head before you hit a breaking point.
- Interpersonal effectiveness. These coping skills help you ask for what you need and say “no” without burning bridges.
Create a customized daily routine with Breeze and make self-awareness a daily habit:
- Create a goal in the app, such as increasing your self-esteem or prioritizing your emotional needs.
- Breeze offers a routine with small steps, such as mindfulness activities, journaling prompts, or mood-boosting exercises.
- Review your daily schedule and cross things off as you complete them.

6. Eye Movement Desensitization and Reprocessing (EMDR)
Bilateral stimulation is the defining characteristic of EMDR. Usually, this is done by watching a therapist’s finger move back and forth or holding buzzers that vibrate in each hand. This rhythmic left-right stimulation mimics what happens during REM (rapid eye movement) sleep. It “distracts” the analytical part of your brain just enough to let the emotional part finally digest the past trauma.
Why does EMDR feel different than talk therapy?
- It involves less talking and more processing. You hold the image in your mind while your eyes follow the movement, letting you feel your feelings in the background.
- The “movie” effect. After a few sets of eye movements, you may notice that your memories begin to feel distant.
- Core belief shifts. You move from “It was my fault” to “I survived it.” Eventually, you may actually feel that shift in your body, not just your head.
Counseling for Trauma: Group Therapy and Expressive Arts
Expressive arts provide an alternative path to healing if you feel like you’ve been talking about your trauma for years, but it’s still “stuck” in your body. Group therapy is the logical choice if you feel isolated and need to know you aren’t alone.
Group Therapy
Group therapy can help you overcome guilt and feelings of chronic trauma. A well-facilitated trauma group offers:
- Universalism. When you hear someone else describe your exact intrusive thoughts, the weight of “being too sensitive” starts to lift.
- Social relearning. A group provides a space to practice setting boundaries and trusting others again.
Expressive Arts Therapy
Not all trauma can be summarized in a conversation. In fact, intense stress often shuts down the verbal centers of the brain, leaving survivors with “wordless” memories such as physical sensations, flashes of color, or sudden shifts in mood. This is where Expressive Arts (Art, Music, Dance, Drama, or Music therapy) comes in.
Why it works for trauma:
- Lowering defenses. Many people find it easier to focus on a physical task, like painting or playing an instrument, than to maintain eye contact with a therapist while discussing a traumatic event.
- Identifying patterns. You might notice themes in your work that you hadn’t been able to put into words yet.
- Physical regulation. Movement-based therapies focus on the body’s “fight or flight” response. They help you learn how to physically calm your nervous system rather than just logically understanding why you’re upset.
Comparing Popular Methods: Is EMDR or CBT Better for Trauma?
Here’s a therapy comparison matrix, explaining which therapies help which trauma symptoms.
| Most effective therapeutic techniques | How does it work? | Best suited for these primary trauma-related symptoms | Limitations | Main Goal |
| Cognitive Behavior Therapy (CBT) | Helps identify negative thoughts and replace the cycle of negative behavior with healthier coping strategies | Cognitive therapy is best for addressing anxiety, depressive episodes, phobias, self-criticism, and intrusive thoughts. | May feel structured or “homework-heavy” for those needing more emotionality | To change trauma-related beliefs and unhealthy behavior patterns formed after a traumatic event and replace them with healthier perspectives. |
| Dialectical Behavior Therapy (DBT) | Combines both acceptance of willingness to change and consequences that are impossible to change | Impulsivity and emotional intensity | Requires long-term commitment and regular practice | To balance acceptance and change while reducing emotional extremes |
| Eye Movement Desensitization and Reprocessing (EMDR) | Reprocesses trauma through bilateral stimulation, for example, eye movements | Post-traumatic stress disorder, complex trauma, and distressing memories | Needs a trained specialist, is emotionally intense | To reprocess traumatic memories so they lose emotional charge |
| Art Therapy | Helps externalize and express emotions in a safer, non-verbal way | Trauma reprocessing, reducing stress, learning to be in a moment | Cannot be a standalone therapy method. Can be ineffective for certain people, especially if clients are (sub)consciously resilient. | To facilitate emotional expression of trauma memory. |
| Group Therapy | Shares a discussion in a guided group setting to cope with personal problems through mutual support | Social anxiety, grief, and feeling lonely | May feel uncomfortable sharing in a group | To build connection and empathy by learning from others’ experiences |
3 Steps to Choose the Right Type of Trauma Therapy
Here’s how you can choose the right trauma therapy:
Step 1: Identify Your Primary Symptoms
The way your trauma “shows up” is the best indicator of where to start.
- If you often feel panic or have anger issues, you need stabilization first. DBT can help you learn to “down-regulate” your nervous system so you don’t feel constantly under attack.
- A body-based approach like expressive arts or somatic experiencing may help you safely reconnect with your physical sensations if you feel lost or numb.
- To help the brain reprocess and “file away” high-intensity memories, flashbacks, or nightmares, try EMDR or prolonged exposure.
Step 2: Consider Your Personal Style
Be honest about how you prefer to communicate. There is no “right” way to heal, only the way that you will actually show up for.
- Do you like structure? If you prefer “homework,” goals, and a predictable schedule, CBT or DBT may feel productive.
- If you’ve spent years talking about your past and it hasn’t helped, look into EMDR or Somatic Experiencing. These therapies require much less verbal storytelling and focus more on brain/body processing.
- Do you need to feel seen? If your trauma involved being abandoned or ignored, group therapy or narrative exposure therapy provides the “witness” you might be seeking.
Try journaling to write down your most common thoughts and group them by topic or request, e.g., “Relationships,” “Hopelessness,” or “Anxiety.” The Breeze app has an in-built journaling feature that will always be available so that you can write down your thoughts as soon as they cross your mind.

Step 3: Check for “Trauma-Informed” Credentials
A recent survey of a thousand Millennials and Gen Z shows that 49% of them have difficulties finding a therapist. On average, participants needed to try at least two therapists before finding the right clinician. Don’t be scared to ask direct questions if you’re unsure how to find a therapist for trauma treatment:
- “What is your specific training in trauma?” Look for certifications in the modalities we’ve discussed.
- “How do you handle it if I get overwhelmed or dissociated during a session?”
- “What is your approach to safety and stabilization before we start diving into past memories?”
Expert Insight
Being truly trauma-informed goes beyond listing trauma modalities on a website. Look for signs that the therapist prioritizes safety and pacing your treatment, and can clearly explain how they work with the nervous system and avoid retraumatization. A trauma-informed therapist should welcome questions, collaborate rather than direct, and adjust treatment based on your capacity rather than pushing insight or exposure too quickly.
Rychel Johnson
Mental health professional
Frequently asked questions
1. What type of therapy is best for trauma?
There is no single “best” trauma therapy, as effectiveness depends on the person and the nature of the trauma. Evidence-based approaches such as trauma-focused cognitive behavioral therapy (TF-CBT), EMDR, and somatic therapies help people process traumatic experiences safely
2. What are the 5 trauma-informed practices?
A trauma-informed approach is guided by five core principles:
- Safety — creating emotional and physical environments where people feel secure
- Trustworthiness — being transparent and consistent in communication
- Choice — respecting autonomy and personal boundaries
- Collaboration — working together rather than exerting control
- Empowerment — supporting strengths, resilience, and self-efficacy
3. What is EMDR therapy for trauma?
EMDR is a structured therapy that helps the brain reprocess traumatic memories so they become less emotionally distressing. It uses bilateral stimulation, such as eye movements, tapping, or sounds, while the client briefly recalls aspects of the traumatic event. This trauma treatment reduces the emotional charge of the memory and allows it to be stored in a healthier way.
4. What does a trauma therapist do?
A trauma-informed therapist helps people understand how trauma affects their thoughts, emotions, relationships, and nervous system. Their role includes creating a safe therapeutic space, teaching grounding and regulation skills, and helping clients to process traumatic memories at a pace that feels manageable. The goal is not to erase the past but to reduce its emotional or psychological harm and restore a sense of control and emotional safety.
Sources
- APA. PTSD Treatments. 2025
- Conti L, Fantasia S, Violi M, Dell’Oste V, Pedrinelli V, Carmassi C. Emotional Dysregulation and Post-Traumatic Stress Symptoms: Which Interaction in Adolescents and Young Adults? A Systematic Review. 2023
- Thriving Center of Psychology. 2024 Mental Health Outlook: Growing Demand for Therapy Among Gen Z & Millennials. December 2023
Disclaimer
This article is for general informative and self-discovery purposes only. It should not replace expert guidance from professionals.
Any action you take in response to the information in this article, whether directly or indirectly, is solely your responsibility and is done at your own risk. Breeze content team and its mental health experts disclaim any liability, loss, or risk, personal, professional, or otherwise, which may result from the use and/or application of any content.
Always consult your doctor or other certified health practitioner with any medical questions or concerns
Breeze articles exclusively cite trusted sources, such as academic research institutions and medical associations, including research and studies from PubMed, ResearchGate, or similar databases. Examine our subject-matter editors and editorial process to see how we verify facts and maintain the accuracy, reliability, and trustworthiness of our material.
Was this article helpful?