Living with childhood trauma can bring its unique challenges. You may live with unstable self-esteem, trust issues, or an insecure attachment style without even understanding that these patterns stem from the past. In fact, two-thirds of U.S. adults experienced at least one adverse childhood experience, which means that there’s a high chance you or your close ones may live with trauma as well. [1]
Further, we’ll explore how traumatic experience can influence your present, the main signs to recognize unresolved childhood trauma, and the most effective approaches to heal it.
What is childhood trauma?
Childhood trauma is a deeply personal experience that results from emotionally painful or overwhelming events during childhood, often leaving a lasting imprint of fear, helplessness, or vulnerability. Two people may experience the same situation, but only one may experience it as traumatic because trauma isn’t just about what happens but also about how we experience and process it. Typically, trauma arises when overwhelming events occur without adequate support, safety, or the presence of a caring adult to help us make sense of them.
For example, when a kid experiences bullying at school and can’t find support from parents or teachers, it can result in chronic stress and a feeling of isolation. As a result, this child can find it difficult to build relationships, rely on others, or feel safe in social situations.
Each case is unique, and what results in a severe trauma for one person may be non-traumatizing for another. Thus, it’s vital to avoid comparing your experience to others’. If you feel that there might be something hidden in your past, it’s worth exploring your experiences and developing new, healthy coping mechanisms.
Examples of adverse childhood experiences (ACEs)
The most common types of childhood trauma can include:
- Neglect. When a child doesn’t get enough attention, care, and support from their parents, it can result in feelings of unworthiness.
- Physical and sexual abuse. Such serious experiences can influence the kid’s ability to regulate emotions and trust the world in general.
- Emotional abuse. Gaslighting, manipulation, and diminishing desires and achievements can also be traumatizing.
- Parentification. When a kid plays the role of a parent in the family, it might interfere with the ability to build healthy relationships in the future.
- Witnessing domestic violence. In case physical safety isn’t guaranteed, a child may develop chronic anxiety.
- Substance abuse in the household. A child’s life might feel dangerous or overwhelming if they stay with a person who lives with addiction.
- Sudden or violent loss of a close person. If there’s no one to support a child and help them process grief, it can turn into chronic pain they carry into adulthood.
Nevertheless, these are only examples, and a person can experience traumatic stress from a wide range of situations beyond the list. Any event that feels overwhelming to the child may result in mental health challenges. It’s also important to recognize that trauma can be shaped by systemic factors such as racism, poverty, or intergenerational trauma, which may complicate or intensify early life adversity.
Emotional vs. physical vs. complex trauma
Traumatic events can take many forms and be different in terms of duration. In short, emotional trauma is about emotional wounds that can leave long-term scars. Physical trauma is more visible, yet it can affect mental state as well. Complex trauma is about long-term harm caused by many difficult events over time.
Here are the most common types necessary to recognize.
| Aspect | Emotional trauma | Physical trauma | Complex trauma |
| Definition | Psychological harm caused by words or manipulative actions. | Physical harm or threat of harm. | Exposure to multiple or prolonged traumatic events |
| Causes | Bullying, verbal abuse, emotional neglect, and witnessing distressing events. | Physical abuse, accidents, natural disasters, and severe illness. | Chronic abuse, neglect, domestic violence, and war. |
| Duration | Can be short-term or long-lasting. | Usually short-term, but can cause lasting consequences if not treated. | Long-lasting condition or series of traumatic experiences. |
How childhood trauma affects adults
Childhood trauma is associated with neurobiological changes that may influence executive function and emotion regulation. It can also increase the risk for dissociation and trauma-related disorders. [2]
This means that if you have traumatic memories, they might have led to certain patterns in adulthood that affect how you think, feel, and relate to others. Here are the most common outcomes.
Emotional and mental health symptoms
Trauma symptoms don’t necessarily appear immediately but can resurface later in life. They might affect your relationships, work, or academic performance, and overall inner balance.
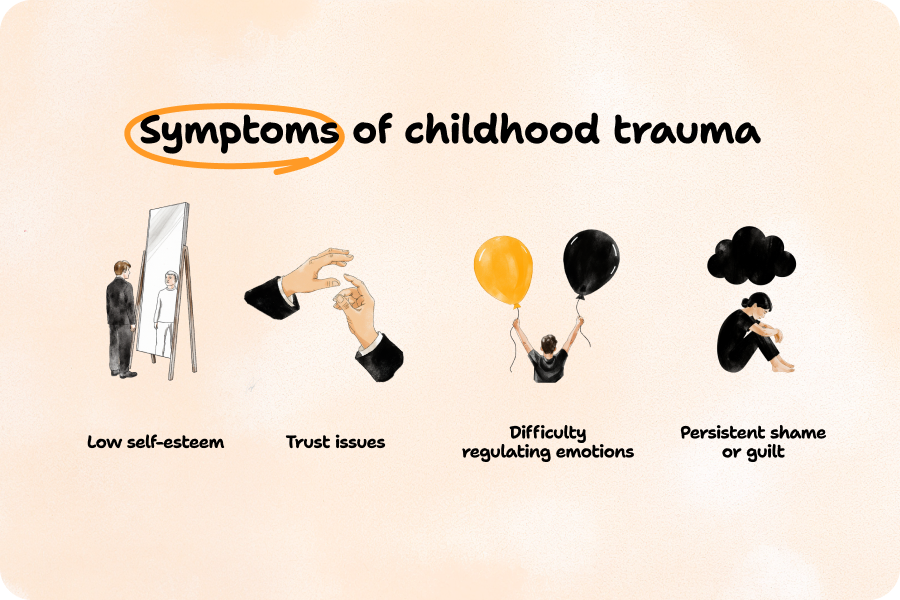
1. Low self-esteem
Child trauma can leave you feeling “I’m not good enough” or “I don’t deserve care and attention.” While it isn’t true, this belief can make you doubt your abilities and avoid opportunities that you may think are “too much for you.”
2. Trust issues
Those who experienced child abuse or emotional neglect may fear intimacy and feel like they can’t trust people anymore. They might always expect to be hurt, which makes it challenging to be vulnerable, open up, and build close relationships.
3. Difficulty regulating emotions
Anger explosions, tears with no clear reason, or anxiety outbursts can follow those who have experienced childhood trauma. This happens because trauma can affect brain areas responsible for managing emotions. When these areas are overactive or underdeveloped due to early stress, it becomes harder to control feelings. [3]
4. Persistent shame or guilt
Guilt complex is another symptom of childhood trauma. It can stem from growing up in a narcissistic family where you felt that you did everything wrong or from being blamed for something outside your control.
Physical health and nervous system impact
Trauma exposure can also bring physical symptoms, as it can be considered a major environmental challenge. [4] In practice, this means that childhood trauma can influence how the nervous system develops and how the body responds to stress further in life. Particularly, it can result in the following:
- Sleep disturbances (insomnia, restless sleep, nightmares).
- Frequent headaches or migraines.
- Gastrointestinal problems (stomach aches, IBS).
- Muscle tension or chronic pain.
- Fatigue or low energy.
- Changes in appetite or weight, which can turn into eating disorders. [5]
Relationship and attachment issues
Mental and physical symptoms of childhood trauma can make it more challenging for people to build long-term and stable relationships. They may choose partners who are emotionally unavailable, have problems trusting others, or are unable to show empathy.
Such people might stay in an abusive relationship because they may believe that “this is what they deserve” or because they didn’t have a healthy role model in childhood.
Even more, when people with childhood trauma start relationships, they might unconsciously push their partners away (because of dismissive-avoidant attachment) or fear losing them (anxious-preoccupied attachment). This can create a cycle of anxiety and distance, which negatively influences building trust in general.
Signs of unresolved childhood trauma in adults
Understanding child trauma is the first step to healing. Still, if you aren’t going to visit a mental health professional right now, there are some signs that can help you spot that you are facing the outcomes of trauma.
Anxiety, depression, and PTSD
Depressive symptoms and other mental health challenges can follow adults with unresolved past trauma. It can interfere with daily functioning and result in higher suicide risks, according to the 2024 study published in the Journal of Affective Disorders.
Even more, people who have experienced trauma may later develop post-traumatic stress disorder, as emotional distress may alter the brain’s memory systems and stress response. Additional symptoms that trauma in adults may bring are:
- Hypervigilance and avoidance behaviors
- Emotional emptiness and numbness
- Self-loathing
- Birthday depression
Self-sabotage, dissociation, or addiction
Findings indicate that there appears to be a relationship between physical neglect in childhood and medically self-sabotaging behaviors in adulthood. [6] These may include neglecting health issues, refusing medical help, or engaging in risky and harmful activities (like reckless driving).
Substance abuse can be another form of self-sabotage. When a person engages in excessive alcohol drinking or drug use, they may try to numb or escape traumatic memories of childhood abuse.
Dissociation or depersonalization can stem from childhood trauma as well. When a kid experiences an overwhelming event, their brain turns on the fight-flight-freeze response. Yet, if there isn’t any possibility to fight or flee, the brain freezes by dissociation to protect the child from emotional pain. The same feeling may follow some people into adulthood, making it challenging to reconnect with their emotions (whether positive or negative).
Patterns of trauma in work, love, and trust
Trauma in adults can manifest in different spheres of life. It may be difficult for such people to trust others or rely on them when they need help. It can lead to hyperindependence and difficulty being vulnerable.
With romantic partners, a person with childhood trauma can hide their real emotions, avoid being fully open, and fear rejection. On the other hand, they might feel afraid that their loved one will leave them and seem too clingy or overly dependent.
At work, such people might exhibit imposter syndrome and constantly doubt their skills. They may constantly overwork to prove their worth or, in contrast, experience procrastination, which can hold back career growth.
How therapy can help heal childhood trauma
Therapy provides a safe space for addressing childhood trauma symptoms and managing related emotions. It helps you develop coping skills necessary to handle traumatic stress from the past and get closer to a happy present.
Key benefits of trauma-informed therapy
- Sense of control. Working with a mental health professional can help you regain the feeling of stability and control over the situation that you lacked in childhood. It empowers you with a feeling of “I can deal with it.”
- Understanding triggers. During the therapeutic process, you will be able to find out what situations, reactions, or people trigger painful memories from the past. Then, you’ll be able to either avoid them or develop strategies to manage these feelings.
- Improved emotional regulation. Behavioral therapy teaches you to react to stressful situations with more self-awareness. You’ll learn to control anger or anxiety much better and avoid feeling overwhelmed.
- Reduced symptoms. Over time, flashbacks, nightmares, and physical stress responses may reduce.
- Better relationships with others. When you start being more in control over your emotions and reactions, your communication with friends, relatives, and colleagues may improve as well.
Have you ever tried working with a mental health professional?
What to expect in childhood abuse therapy sessions
Treating childhood trauma is a complex process that requires engagement and trust from both a mental health professional and a patient. During sessions, you might need to:
- Share your story.
- Analyze your emotions and feelings.
- Identify patterns that stem from trauma.
- Learn coping strategies for managing stress, anxiety, or flashbacks.
- Practice emotional regulation techniques.
- Explore and challenge negative beliefs about yourself.
- Rebuild trust and boundaries in relationships.
- Set personal goals for growth and healing.
The approach to work can vary greatly based on the approach you choose. However, whatever type of trauma therapy you choose, you can often expect a supportive place to share what’s inside and a professional who can always help you find the way out of traumatic memories.
How long does it take to heal an early childhood trauma?
There’s no clear answer for how long it takes to heal unresolved childhood trauma. Each case is unique and depends on many factors, such as the severity of the trauma, the age at which it occurred, and personal coping mechanisms. The fact that a person lives with other mental health conditions or experiences PTSD symptoms also matters.
In addition, the process might be nonlinear because old wounds can resurface at different stages of life. Yet, over time, you’ll learn to build resilience, and the healing process will become less focused on the pain from the past and more about building your happy and fulfilling future.
Abigail Fernald, LCSW, explains how a patient can accept a nonlinear process of healing and recognize progress even when difficult emotions arise. “Healing from trauma is rarely a linear journey; it often involves revisiting emotions, memories, or patterns that resurface as we grow. Patients can begin to accept this nonlinearity by reframing setbacks as part of the process, not failures. In therapy, we often emphasize that experiencing painful emotions is not a sign of regression, but rather an indication that deeper layers of healing are unfolding. It’s also helpful to celebrate small shifts, such as increased awareness, self-compassion, or the ability to pause before reacting, as meaningful progress. Journaling, tracking patterns, and receiving consistent reflection from a therapist can help clients recognize how far they’ve come, even when the path feels hard. Ultimately, honoring each step as valid supports resilience and sustained growth.”
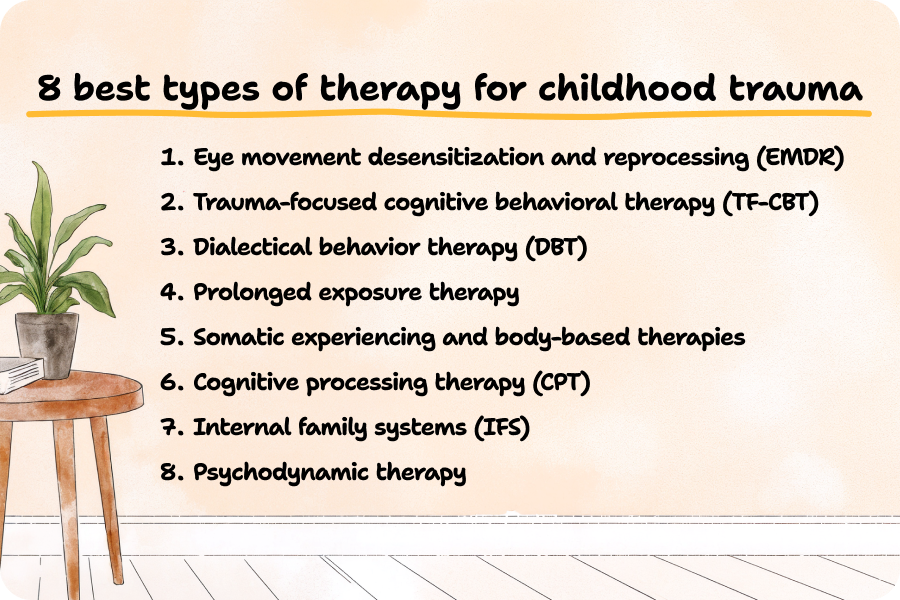
8 best types of therapy for childhood trauma
There are many treatment options that can help you heal from traumatic events. Still, everyone should choose what works best for them, as no single approach fits all.
Before beginning trauma processing, it’s essential to ensure a foundation of emotional safety. Many trauma-informed therapists start by helping clients build tools for stabilization, such as grounding, breathwork, or mindfulness, so that the healing journey feels manageable and not re-traumatizing.
1. Eye movement desensitization and reprocessing (EMDR)
This is a structured approach tailored for treating post-traumatic stress disorder and trauma-related conditions. During treatment, patients need to move their eyes in a specific way while focusing on a traumatic memory. Eye movement desensitization and reprocessing can also involve other ways of bilateral stimulation, such as alternating sounds, gentle tapping, or tactile sensations.
This allows our brain to reshape past events and reduce the distress associated with them. In fact, 7 of 10 studies reported EMDR therapy to be more rapid and/or more effective than trauma-focused cognitive behavioral therapy. [8]
2. Trauma-focused cognitive behavioral therapy (TF-CBT) as part of cognitive behavioral therapy (CBT)
This is a well-known and evidence-based treatment model that applies trauma-specific and behavioral techniques to overcome painful memories and develop coping mechanisms. During sessions, a specialist works with traumatized children and their non-abusive caregivers to create a safe environment and help them process past wounds.
Trauma-focused cognitive behavioral therapy (TF-CBT) is often structured and time-limited, but the number of sessions can vary based on individual needs. While many treatment models are designed for 8–25 sessions, some people may benefit from a shorter or longer duration. TF-CBT can be offered on its own or integrated into a broader course of therapy for children and adults navigating childhood trauma.
3. Dialectical behavior therapy (DBT)
Originally developed as a type of cognitive behavioral therapy for borderline personality disorder and suicidal tendencies, DBT may also be helpful to treat PTSD and trauma in adults. It focuses on teaching mindfulness, emotion regulation, and distress tolerance.
Structured sessions help people overcome self-sabotaging behaviors after experiencing childhood abuse. You may need to practice exercises provided by a therapist during and between sessions to gradually develop skills that will let you manage emotions better.
4. Prolonged exposure therapy
PE is another type of cognitive behavioral therapy that is tailored to treat PTSD symptoms and the consequences of traumatic events, particularly childhood trauma exposure. Prolonged exposure therapy allows people to safely explore trauma-related memories they might have been avoiding. This repeated, controlled exposure helps reduce fear and anxiety over time and helps adapt to the triggers so they no longer disturb daily functioning.
5. Somatic experiencing and body-based therapies
This approach helps process trauma in adults through releasing the body’s stored stress response. Through breathwork, movement activities, yoga, dance therapy, and guided meditation, people can address unprocessed memories related to the past.
During sessions, you may need to focus on bodily responses and can experience tension, warmth, tingling, or any other feelings. This process can help build physical awareness and allow the nervous system to return to a state of balance.
6. Cognitive processing therapy (CPT)
This is a more universal approach that may help people treat PTSD and childhood trauma, as well as challenge unhelpful thoughts and negative beliefs about themselves in general. Cognitive processing therapy is also used to address co-occurring issues such as substance abuse, depression, or anxiety.
A mental health professional can ask you to do specific exercises to find out how trauma affects your emotions and behavior. Within cognitive processing therapy (CPT) treatment, you may also need to fill in specific worksheets, practice challenging negative thoughts at home, and improve self-awareness through discussion.
7. Internal family systems (IFS)
This approach views the mind as something made up of different “parts,” each with its own roles and perspectives. During the healing journey, the goal of the client is to find wounded parts, “hear” them, and learn to approach them with compassion.
It combines the process of healing with trauma-sensitive interventions that allow people to build resilience in the long run. When you build healthier relationships with all inner “parts,” you can experience greater emotional balance and handle past wounds much better.
8. Psychodynamic therapy
This is a type of talking therapy for addressing childhood trauma that allows people to spot unconscious thoughts and behavioral patterns that stem from past experiences and change them for more nurturing ones. Patients are encouraged to use free associations, interpretations, and defense mechanism exploration, which helps bring unconscious feelings and improve self-awareness.
Finding the right therapist
“How to find a therapist?” is an even more important question than deciding on a modality in your healing journey. The therapeutic relationship is the key to successful treatment, and many therapists are trained in numerous modalities, enabling them to help clients navigate which modality will be the best fit for them.
Questions to ask a trauma therapist
A quick contact before the first actual session can save you time and help you find a specialist who resonates with you most. This is what you may need to ask them:
- Do you have experience helping adults with trauma?
- What therapy methods do you use for trauma?
- How do you make sure sessions feel safe?
- How do you help with strong emotions or triggers?
- How will we know if therapy is helping?
- How do you protect my privacy?
- How often should we meet, and how long does therapy usually last?
- What happens if I have a setback or feel worse during therapy?
Credentials to look for
Expert Insight
“When seeking a therapist for childhood trauma, it’s important to look for a licensed mental health professional, such as an LCSW, LPC, LMFT, or psychologist with experience in trauma-focused therapy. Additional certifications in evidence-based trauma modalities, such as EMDR (Eye Movement Desensitization and Reprocessing), TF-CBT (Trauma-Focused Cognitive Behavioral Therapy), etc., can indicate specialized training. You might also look for therapists who describe themselves as trauma-informed or who have completed trainings in somatic therapies, Internal Family Systems (IFS), or polyvagal theory. A strong trauma therapist will emphasize safety, collaboration, and choice, and will be open to discussing their approach with you. Most importantly, the therapeutic relationship itself should feel validating, respectful, and attuned to your pace and needs.”
Abigail Fernald
Mental health professional
Online vs. in-person therapy
Studies prove online therapy is as fruitful as traditional treatment options. [7] Yet, there’s no clear answer as to which is better: online or in-person treatment. Everyone can choose what’s more effective for them. Here’s a quick comparison of the main aspects.
| Online Therapy | In-Person Therapy |
| Can be accessed from anywhere with Internet, ideal for people living in remote areas or having busy schedules. | Requires travel to the therapist’s office and may be limited by location. |
| Offers the comfort of being in your own space; you may feel safer sharing sensitive topics. | Provides a private space outside the home, which can help clients separate therapy from daily life. |
| Can feel slightly less personal, as body language may be harder to read. | Has a stronger in-person connection because the therapist can notice body language and nonverbal cues. |
| More flexible. | Less flexible because sessions must fit office hours and travel time. |
| It can be less expensive, as you may find a professional from anywhere in the world. | It may be more expensive. |
Getting the most out of therapy
To increase the efficiency of mental health services, it’s essential to approach them responsibly and put in effort both during sessions and in between them. This is what you can do to make cognitive behavioral techniques more effective.
Building trust and safety
First and foremost, it’s essential to establish trusting communication with a therapist. You need to understand that during sessions, your emotions are vital, respected, and won’t be judged. To feel more comfortable during treatment, you can try:
- Share specific fears with your therapist before starting healing or during it.
- Agree on topics that feel safe to discuss first.
- Request breaks during sessions if you feel overwhelmed.
- Identify personal goals for therapy and share them with your therapist.
- Communicate any discomfort with exercises or homework tasks.
Journaling and between-session practices
When treating trauma or any mental health conditions, it can be helpful to track your reactions and triggers between sessions. The Breeze app allows you to:
- Improve self-awareness through self-discovery tests. With more than 30 assessments, you can find out a lot of new things about your reactions, personality traits, and approach to life. In addition, Breeze provides you with tailored tips to manage stress and reinforce resilience.
- Track your mood and notice reactions. Advanced mood tracker and journaling options help you collect insights on your emotions and reflect on progress over time. Over time, you can discuss these patterns with your therapist and adjust the treatment process if needed.
- Regain inner balance. Relaxation games can become another way to feel better after a tough day or an insightful session. They allow you to get more mindful, focus on what’s happening inside, and take care of your inner child.
Tracking progress and setbacks
Regularly monitoring changes in how you approach your past and life in general can help you stay motivated and ensure that you move in the right direction. Here are some tips to notice your progress and overcome tough times:
- Accept that setbacks might happen, and it’s completely normal.
- Note specific situations where coping strategies worked or didn’t.
- Track improvements in sleep, mood, or stress levels.
- Set measurable goals and mark when you achieve them.
- Record recurring negative beliefs.
- Share observations with your therapist to adjust your treatment plan if necessary.
Can you ever fully heal from childhood trauma?
The answer highly depends on the person themselves and the nature of the trauma. For many people, it’s possible to reduce the intensity of painful memories and improve overall mental health. It isn’t about getting back to the time when you didn’t have trauma. Instead, healing means learning to live fully despite the past.
Frequently asked questions
How do I know if I have childhood trauma?
- Analyze your past and remember what traumatic events you might have experienced.
- Think about whether you experience the symptoms of an unresolved childhood trauma.
- Take Breeze’s childhood trauma test and discover whether you live with hidden patterns that stem from a traumatizing experience.
- Visit a mental health professional who will conduct a comprehensive assessment and help you find out more about your well-being.
Is childhood trauma treatment worth it?
Yes, childhood trauma treatment will help you overcome trauma-related symptoms or handle them better and develop the coping skills necessary to navigate daily challenges. If you approach the healing process seriously, after some time, you may notice gradual but noticeable improvements in your relationships with others, emotional regulation, and overall level of happiness.
How long does addressing childhood trauma take?
Treating childhood trauma may require months or even years. The healing journey and its duration are unique for everyone and may depend on the symptoms, co-occurring mental health conditions, treatment consistency, support from close ones, and the complexity of the trauma.
What is the new therapy for childhood trauma?
There’s no single new or unique approach that can help you overcome traumatic childhood experiences. Instead, each person can find healing through different evidence-based methods. Eye movement desensitization and reprocessing (EMDR) and trauma-focused cognitive behavioral therapy (TF-CBT) can be considered as a few of the most effective ones.
Sources
- Swedo EA, Aslam MV, Dahlberg LL, et al. “Prevalence of Adverse Childhood Experiences Among U.S. Adults — Behavioral Risk Factor Surveillance System.” 2011–2020. MMWR Morb Mortal Wkly Rep 2023;72:707–715.
- Cross D, Fani N, Powers A, Bradley B. “Neurobiological Development in the Context of Childhood Trauma.” Clin Psychol (New York). 2017
- Cimeša, Mladen & Sokić, Aleksandra & Cimeša, Božana. (2023). “Childhood Trauma and its Effect on Brain Development: Neurobiological Mechanisms and Implications.”
- McFarlane AC. “The long-term costs of traumatic stress: intertwined physical and psychological consequences.” World Psychiatry. 2010
- Cay M, Gonzalez-Heydrich J, Teicher MH, van der Heijden H, Ongur D, Shinn AK, Upadhyay J. “Childhood maltreatment and its role in the development of pain and psychopathology. Lancet Child Adolesc Health.” 2022
- Sansone, Randy & Wiederman, Michael & McLean, Jamie. (2008). “The Relationship between Childhood Trauma and Medically Self-Sabotaging Behaviors among Psychiatric Inpatients.” International journal of psychiatry in medicine.
- Verma, Gobind. (2023). “Online Therapy and its Effectiveness in the Treatment of Mental Disorders.”
- Shapiro F. “The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences.” Perm J. 2014
Disclaimer
This article is for general informative and self-discovery purposes only. It should not replace expert guidance from professionals.
Any action you take in response to the information in this article, whether directly or indirectly, is solely your responsibility and is done at your own risk. Breeze content team and its mental health experts disclaim any liability, loss, or risk, personal, professional, or otherwise, which may result from the use and/or application of any content.
Always consult your doctor or other certified health practitioner with any medical questions or concerns
Breeze articles exclusively cite trusted sources, such as academic research institutions and medical associations, including research and studies from PubMed, ResearchGate, or similar databases. Examine our subject-matter editors and editorial process to see how we verify facts and maintain the accuracy, reliability, and trustworthiness of our material.
Was this article helpful?