Complex post-traumatic stress disorder (CPTSD) and borderline personality disorder (BPD) are easy to confuse when you’re self-diagnosing. I’m Emily Mendez, a former therapist who wants to help you make sense of things.
Do you have questions about CPTSD vs. BPD as you try to understand your own thoughts and behaviors? Complex PTSD and borderline personality disorder are similar on the surface.
However, these are two distinct conditions. Treatment protocols can also be vastly different. That’s why working with a trained therapist for CPTSD or BPD is essential.
Is Complex PTSD Similar to BPD?
Yes! That’s why figuring out if you have CPTSD or BPD can be difficult. Both are serious mental health conditions. Both also primarily revolve around difficulties with self-regulation.
Another factor that can make it even more difficult to tell the difference between CPTSD and BPD is that both are often rooted in trauma.
With that in mind, a look at childhood trauma statistics in 2024 makes it easy to see why diagnoses for both are on the rise.
Let’s start the complex PTSD vs BPD conversation with solid definitions.
Complex PTSD is a condition that can occur following multiple or ongoing traumatic experiences. This is a different conversation than PTSD vs BPD.
PTSD might be caused by a single traumatic event. Think warfare or devastating accidents. CPTSD might be caused by an ongoing childhood of abuse and instability.
CPTSD is generally rooted in any kind of chronic trauma a person couldn’t escape.
As a result, they no longer feel safe. Their worldview and self-facing view are skewed. A person may also suffer from flashbacks and nightmares. I’ll get into more common CPTSD symptoms further down.
BPD is a personality disorder. A person with BPD struggles with an unstable self-image and feelings of emptiness. It’s not really fair to make a comparison of BPD vs. trauma because BPD is often a response to trauma. It just displays differently.
Is there a quick do I have BPD or CPTSD test? Not exactly. However, there are some general ways to know the difference between CPTSD and BPD.
I recommend finding good books on BPD or learning about the 17 symptoms of complex PTSD to start.
Next, let’s break down the symptoms of borderline personality disorder vs complex PTSD.
CPTSD vs. BPD
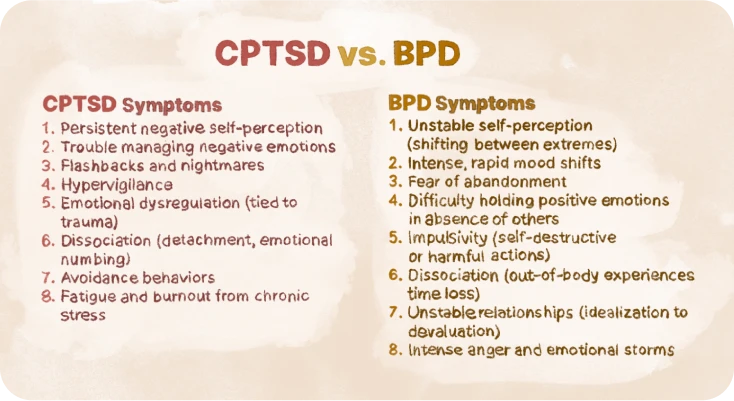
One of the best ways to differentiate between CPTSD vs. borderline is to look at symptoms. I’m going to list the most prominent ones to show you both overlaps and differences.
1. Self-perception
Here’s one of the biggest differentiators when determining CPTSD or BPD. Both involve skewed self-perception. CPTSD involves persistent negative self-perception. While it’s harmful, it’s consistent. With BPD, a person’s self-perception can be all over the map.
They can go from believing they are superior to feeling shamefully inferior based on the situation. Their unstable self-view can cause a person with BPD to act chaotically. They may even have contradictory self-views.
2. Emotional dysregulation
The mood is tough with CPTSD versus BPD because both share emotional dysregulation. However, this core symptom manifests differently for BPD vs CPTSD.
People with CPTSD have trouble managing negative emotions. They can get into spirals. They can even act out or engage in harmful behaviors. Depression and anxiety are ever-present dangers.
With BPD, mood shifts can be massive and volatile. A person with BPD may go from “loving” someone to “hating” them in the blink of an eye.
They also switch between idealizing and vilifying quickly. Mood changes can last hours or days. In addition to giving people around them emotional whiplash, these emotions can cause general instability.
They can be accompanied by impulsive decisions. Common emotional storms experienced by people with BPD involve uncontrolled anger, hatred, sadness, fear, and anxiety. Alternatively, they can also act out with intense love.
3. Impulsive behaviors
One difference between BPD vs. CPTSD is “acting out.”
Generally, people with CPTSD don’t have impulsive actions or self-destructive behaviors. However, impulsivity can be present with CPTSD.
Meanwhile, impulsivity is a steady hallmark of BPD. People with BPD will both literally and figuratively “blow things up.” They will burn bridges in the blink of an eye.
This goes for everything from quitting a job to ending a relationship. Impulsive behaviors are sometimes used to harm others. Think “destroying property” or “telling lies about someone.”
However, they are usually self-destructive. This ties in with people with BPD being at increased risk for drug use. Self-harm is also considered a pervasive problem among people with BPD.
4. Flashbacks
One of the more confusing things about CPTSD vs. PTSD is that both can involve flashbacks. In general, flashbacks with PTSD are more focused on the traumatizing event. CPTSD survivors may not have a single focal point to flashback to.
As a result, their flashbacks may be focused more on familiar feelings. However, traditional flashbacks can certainly take place.
What does a CPTSD flashback feel like? It can feel like the past is happening in the present moment. The most obvious way is through an image, sound, or physical feeling. You might also experience the emotions that occurred during the initial trauma.
For example, someone who was belittled throughout childhood by a parent may feel intense shame come over them. Fear and sadness are also common feelings.
When childhood emotional neglect is a trigger, flashbacks could come in the form of despair. During a flashback, staying connected with reality can be challenging.
Not everyone with CPTSD lives out the trauma through flashbacks. Some people who have recurring nightmares don’t realize this is a CPTSD manifestation. Like flashbacks, nightmares may be focused on specific sensations or emotions.
This is where another big difference between CPTSD and BPD happens.
Flashbacks and nightmares aren’t symptoms of BPD. Generally, trauma manifests as emotional distress and intrusive thoughts instead of “experiences.” A person with BPD may live out the trauma through a distorted sense of self instead of vivid memories.
Caveat time! This can’t be a standalone symptom for determining borderline personality disorder vs CPTSD. Some people with BPD do experience flashbacks.
There are people who have co-occurring BPD and PTSD. A review from 2021 shows that somewhere between 30% and 70% of adults with BPD have also had PTSD at some point.
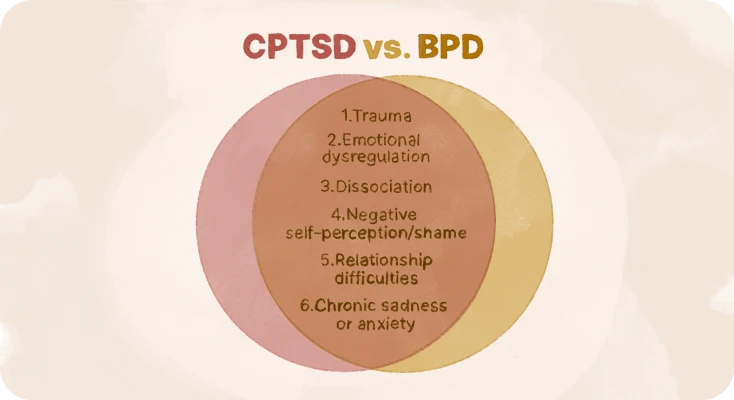
5. Disassociation
One thing that defines BPD is dissociation. What is it? Disassociation is the act of detaching from yourself or your surroundings.
When we detach from ourselves, this is also called depersonalization. When we float away from our surroundings, it’s called derealization.
While occasional dissociation can be normal, chronic dissociation is a classic BPD symptom.
Here are some symptoms of dissociation with BPD:
- Feeling like you aren’t real.
- Feeling like the world around you isn’t real.
- Having an out-of-body experience.
- Wondering if you are a different person.
- Feeling emotionally numb.
- Feeling little to no physical pain.
- Losing time.
- Having tunnel vision while completing tasks.
- Hearing voices.
- Arriving somewhere without knowing how you got there.
- Feeling time moving “differently” for you.
- Becoming immobile or incapacitated with no physical cause.
- Having difficulty distinguishing between reality and fantasy.
What does dissociation feel like for someone with BPD? The experience can differ by person or situation.
Many of my clients with BPD dissociation report feeling like they are outside of their bodies. Some claim they’ve been able to “float above a room” to watch themselves. Others describe it as a kind of cognitive dormancy. They might simply show up someplace without remembering how they got there. Others experience a feeling of extreme detachment that makes them forget the details of their own lives.
I want to make it clear that dissociation isn’t exclusive to BPD. It can be present with psychosis. People with dissociative identity disorder (DID) and schizophrenia also frequently experience dissociation.
6. Hypervigilance
Do you feel like you can never “settle down” because you’re living with hypervigilance? It’s a consequence of the fight-or-flight state going into overdrive. Many people with CPTSD live with hypervigilance as a result of trauma.
While hypervigilance may seem like a “superpower” on the surface, it’s taxing. The nervous system is constantly scanning for “danger.” The body’s senses create alarm bells over every sound and sight.
Unfortunately, this chronic state of arousal can leave us fatigued. It’s common for people with CPTSD to experience severe burnout. You may struggle to fall asleep. Relaxing can also be impossible.
As a result, people with hypervigilance are often edgy. Here are some signs you’re dealing with hypervigilance:
- You’re always overestimating danger.
- You catastrophize situations by assuming the worst at all times.
- You are easily startled. For example, the sound of your dog getting up across the room could send you jumping out of your chair.
- You have a high heart rate, elevated blood pressure, and dilated pupils.
- Your fear of the threat of danger causes you to avoid situations or places obsessively.
Abuse, emotional neglect, or physical neglect left your mind and body fearful. Your hypervigilance is your body’s way of attempting to detect the threat this time.
7. Emotional Impermanence
Why am I so emotional when my partner isn’t with me? This is another telltale BPD symptom that generally doesn’t carry over to CPTSD. It’s also one of the reasons why people with BPD often find themselves in extremely volatile relationships. This explains why so many people with BPD get “clingy” in relationships.
What does emotional impermanence mean? The simple answer is that it’s the opposite of emotional permanence.
This refers to the ability to hold on to positive feelings from a relationship even when you’re not physically present with someone. You know you’re loved. You know you love them. The awareness of the love remains even when distance or arguments creep in.
Emotional permanence is what allows us to have healthy, stable relationships as we weather the ups and downs of life.
For people with BPD, emotional impermanence makes every day feel like a big question mark. It’s the feeling that we can’t be certain that someone still loves us if they’re not standing in front of us.
This “scariness” of it makes people with BPD lash out at loved ones. They may feel the need to be clingy or “test” loved ones. Often, they feel anxious and uneasy in relationships.
Unfortunately, these desperate behaviors can turn people off. This can create a self-affirming spiral that reinforces a sense of being unlovable.
People with CPTSD don’t experience this. While they may feel unworthy or unlovable, they can generally understand that feelings can exist outside of direct contact.
8. Onset
When symptoms occur, there is another big difference between CPTSD vs. BPD. Generally, a personality disorder forms at or before adolescence.
If you don’t have symptoms by the time you graduate high school, it’s unlikely that you have BPD. Meanwhile, complex PTSD can develop at any time.
Most people begin to experience symptoms by adolescence if their CPTSD is a result of ongoing childhood trauma or childhood emotional neglect.
Treatment for C-PTSD vs. BPD
Treatment modalities for complex PTSD vs. BPD can vary based on severity. In many cases, some treatments can overlap. How do you actually treat BPD vs. trauma?
For CPTSD, practitioners often start at the root with trauma-focused therapy. This usually begins with something called trauma-focused cognitive behavioral therapy (TF-CBT), which is a targeted form of CBT. It can help a person to reroute their beliefs and behaviors.
For those who don’t get what they want from CBT, eye movement desensitization and reprocessing (EMDR) therapy shows lots of promise for people trying to overcome trauma.
For people with CPTSD struggling with trauma-related memories, exposure therapy may allow them to learn that triggers aren’t necessarily dangerous cues that require avoidance.
On another hand, with BPD, talk therapy is considered the gold standard. Some people with BPD also require medication to help them begin to stabilize their mood and behaviors.
Dialectical behavior therapy (DBT) and schema therapy are also commonly utilized for BPD. Both are potentially effective because they help to increase self-awareness. By syncing with emotional responses, people with BPD can learn to manage their intense emotions instead of acting out.
FAQ
Can you have both C-PTSD and BPD?
Yes, this is called a dual diagnosis. If you’re not sure if you have CPTSD or BPD because you’re experiencing all of the symptoms above, it’s possible that you have both. It’s important to work with a psychiatric professional with an understanding of the comorbidity of the two.
How do I know if I have CPTSD or BPD?
Consider taking a borderline personality disorder test to help you determine where your symptoms skew with complex PTSD vs borderline personality disorder. The truth is that telling the difference isn’t always easy.
For example, it can be almost impossible to tell the difference between quiet BPD vs. CPTSD if you’re not acting out. Quiet BPD is a more subdued form of BPD where you internalize emotions. It lacks the “chaos” of traditional BPD from the outside.
Mood swings, fear of abandonment, and erratic feelings are “stuffed down” and internalized. The only way to differentiate between complex PTSD vs. borderline is to be evaluated by a therapist.
What is the difference between complex PTSD vs. BPD?
Complex trauma vs. BPD comes down to type. Complex PTSD is a mental health condition that develops in response to trauma. BPD is a personality disorder. Mental health disorders impact your mood, thoughts, and behaviors.
With a personality disorder, you’re deeply entrenched in long-term thought patterns that impact self-perception and outward actions. While both can be destructive, BPD generally leads to more chaos and harm compared to complex PTSD.
Disclaimer
This article is for general informative and self-discovery purposes only. It should not replace expert guidance from professionals.
Any action you take in response to the information in this article, whether directly or indirectly, is solely your responsibility and is done at your own risk. Breeze content team and its mental health experts disclaim any liability, loss, or risk, personal, professional, or otherwise, which may result from the use and/or application of any content.
Always consult your doctor or other certified health practitioner with any medical questions or concerns
Breeze articles exclusively cite trusted sources, such as academic research institutions and medical associations, including research and studies from PubMed, ResearchGate, or similar databases. Examine our subject-matter editors and editorial process to see how we verify facts and maintain the accuracy, reliability, and trustworthiness of our material.
Was this article helpful?





